
Solving the Puzzle – Excisional vs Shave Biopsy
Dermatologists have a few tools in their medical bag when it comes to solving the mystery of lesions on the body. Sometimes there is confusion as to why one type of biopsy is used over another. (In fact, today’s post was inspired by to a curious patient!) So, what’s the deal with biopsies?
There are two ways to biopsy lesions to ensure that they are not melanoma- excisional biopsy and incisional biopsy.
The National Comprehensive Cancer Network (NCCN), American Academy of Dermatology (AAD), American Joint Committee on Cancer (AJCC), British Association of Dermatologist, and many other professional groups have stated that the ideal method of biopsy is a full thickness excision either by punch or scalpel. However, some dermatologists and many primary care physicians do not chose this method to biopsy lesions to rule out melanoma. Why?
Advantages of Excisional Biopsy
Why do you need to remove the whole mole?
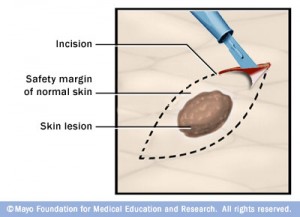
The reason we are removing the lesion is for the pathologist to examine it and determine if it is melanoma. It is not uncommon for melanomas to arise in pre-existing moles and for much of the mole to still be entirely benign. Removing the entire lesion and sending the whole thing to the pathologist is the only way to ensure that the pathologist has the best opportunity to make the correct diagnosis.
For this reason, it is only in extraordinary circumstances that I take a partial sampling of a mole. If I can’t get the whole mole out with reasonable margins using a punch excision technique, we have the patient return to excise the whole thing. However, if I believe the lesion is a melanoma, I always try to excise the lesion on the spot, no matter how big so that we can get the diagnosis ASAP.
What about just biopsying the ugliest part of it?
If the mole is cancerous, meaning that it is a melanoma, the single most important factor is the measurement of how deep it is in the skin (the Breslow Depth). This depth determines how wide the margin of excision needs to be to treat it as well as determining whether you should consider a procedure called a Sentinel Lymph Biopsy to see if the melanoma has started to spread. Depth is the single best predictor of survival.
When moles have been partially sampled and found to be melanoma, you have to go back and do a second procedure (called microstaging) to ensure that no other part of the lesion has melanoma deeper than what you have already found. 20% of the time, the diagnosis is “upstaged” because the initial sample missed the most crucial portion of the tumor. The consequence can be mis-staging and delays in implementing the correct treatment plan.
Depth is Essential
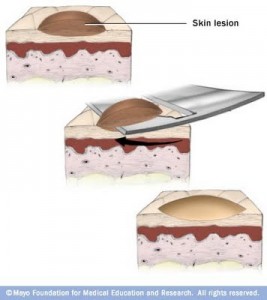
One biopsy method that can lead to a less-than-optimal pathology specimen is a shave biopsy. In this biopsy technique a razor is moved across the skin creating a wound similar to a golf divot. Unfortunately, performing shave biopsies, while seemingly simple, is actually technically quite difficult. The performing provider must ensure that the ‘divot’ is deep enough. Frequently, however, the shave transects, or cuts through, the base of the tumor leading to mistakes with staging and subsequent treatment. If the lesion has been fully excised to begin with, using a full thickness excision like a punch excision or an excision with scalpel, the problems with transecting the tumor disappear.
The problem of recurrent nevi
When moles are incompletely removed by shave biopsy they often grow back and are referred to as recurrent nevi. They tend to look worrisome to the clinician. This often prompts a repeat biopsy and/or excision. Unfortunately, due to scar tissue formation from the original partial remove, the microscopic appearance of the recurrent nevus can be quite alarming – even to the point of being misdiagnosed as a melanoma despite being a benign tumor. This can be a huge problem down the road for people who have had many shave biopsies. For this reason, when moles are incompletely removed by shave biopsy, you often have to go back and excise whatever is left behind.
If the initial growth was removed via an excisional technique the rate of recurrence is minimal.
Why do a shave biopsy to diagnose melanoma?
Usually the argument is that it works most of the time, or that its faster and you can see more patients in a day if you just do shave biopsies. However, generally shave biopsies lead to more costs and diagnostic errors than they prevent. There are certain circumstances where a deep scoop-shave biopsy, or a very large and broad shallow shave biopsy may be reasonable, or even preferable, but only in the most experienced of hands should they be considered.
Do it right or do it twice
When the diagnosis is in doubt regarding a mole or growth you want to ensure that you obtain an accurate diagnosis as quickly as possible. Excisional biopsies are the best way to ensure accurate diagnosis and staging of the tumor so that further treatment can be planned.
When are shave biopsies useful?
When you don’t need to go deep into the skin to ensure an accurate diagnosis like you need to do for melanomas, a shave biopsy often leaves a very small scar if any at all. This makes shave biopsies very useful for diagnosing tumors that arise in the top layer, or or epidermis of the skin, such as basal cell carcinoma or squamous cell carcinoma.
If you think you may need a skin biopsy (or someone you love may need one), call today at (425) 654-1275 for a skin cancer screening. It is a quick appointment and can put your mind at ease.



No Comments
Sorry, the comment form is closed at this time.